Can We Kill Antibiotic-Resistant Superbugs?
Table of contents

Superbug. It sounds like the name of Ant-Man’s sidekick or a one-hit wonder English rock band from the 1970s. But superbugs might just pose the greatest threat to humanity outside of killer asteroids, invading aliens, secret Nazi bases in Antarctica or the latest YouTube social media challenge for kids. Seriously, though, the rise of antibiotic-resistant microbes might be reason enough to trade that bunker filled with a year’s worth of cocktail weenies for a “boy in the plastic bubble” containment system to save yourself from the next deadly infection outbreak. And where there’s potentially catastrophic danger to the survival of the human race, there’s money to be made. Let’s dive into the world of superbugs.
What is a Superbug?
Once upon a time (somewhere around the turn of the 20th century), illnesses such as pneumonia, tuberculosis, and diarrhea were responsible for about a third of all deaths in the United States, according to the U.S. Centers of Disease Control (CDC). These infections are caused by bad bacteria and other miscreant microorganisms. Today, the top spots have been taken by other diseases such as cancer and heart disease, largely thanks to the development of antibiotic medicines such as penicillin beginning in the 1940s. Now, a half-century later, the overuse of these same antibiotics is one of the main causes behind the rise of superbugs – bacteria that have evolved resistance to drugs, proving the maxim that whatever doesn’t kill you makes you stronger.
Some Superbug Statistics and Stories
About two million people in the United States get an antibiotic-resistant infection, and at least 23,000 of those people die each year, according to CDC. Worldwide, the number of deaths is about 700,000, according to the World Health Organization (WHO). Those numbers are expected to jump to 10 million people per year by 2050 if nothing is done to stop the spread of these superbugs.

In India, which is on the front lines of the superbug super war, such suped up bacteria kill nearly 60,000 newborns every year, Bloomberg reported in an article about some of the homegrown startups that are waging war on superbugs. In one study, Bloomberg reported, half the patients in a single South India hospital got at least one infection during their stay, with three-quarters of those showing resistance to multiple drugs. A New York Times article earlier this year said the next superbug could come from war-torn Yemen, where antibiotic use is akin to opioid use in the United States. You might recall from history class – for those of you who didn’t skip out for an early-afternoon bong hit – that the biggest killer during the American Civil War wasn’t bullets but infections. The same thing is happening in Yemen in 2018.
The Superbugs Hit List
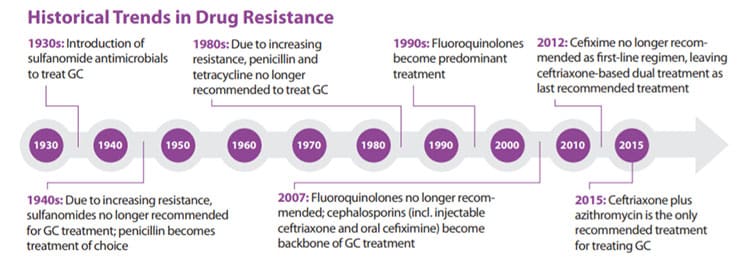
Both the CDC and WHO have put out their own versions of the FBI’s Most Wanted List, detailing the biggest and baddest bacteria out there today. The CDC published its list of the top 18 antibiotic-resistant threats in 2013. WHO followed suit in 2017 with a catalog of 12 families of bacteria that pose the greatest threat to human health. Among the supervillains of bacteria is the so-called “phantom menace” of bacteria known as Enterobacteriaceae, which can cause a deadly infection and is resistant to all known antibiotics, including big guns like a family of antibiotics known as carbapenems. One form of the carbapenem-resistant Enterobacteriaceae (CRE) can even spread its resistance to other bacteria. Also making it to the top of both lists is the bacteria Neisseria gonorrhoeae, which causes the sexually transmitted disease gonorrhea. Below are the lists from the CDC and WHO.

As you can see, both agencies have generated lists with somewhat different priorities, as the CDC is specific to the United States, while WHO is concerned with the bigger planetary picture, where vaccines may exist but aren’t necessarily available in some parts of the world. Among the most dangerous are those groups of multidrug-resistant bacteria that hang out in places like hospitals and nursing homes such as Escherichia coli (E. coli), which falls under the Enterobacteriaceae crime family. Most of these bacteria are gram-negative bacteria, referring to a stain test developed back in the 19th century for classifying different types of bacteria based on a chemical stain.
Money for the War on Superbugs
The prospect of a worldwide, superbug-led epidemic has helped open the floodgates on money to fight the problem. One of the biggest spenders is a non-profit public-private partnership called CARB-X, for Combating Antibiotic Resistant Bacteria. CARB-X has more than $500 million in its coffers to fund its own portfolio of what it calls the “world’s largest early development pipeline of new antibiotics, vaccines, rapid diagnostics, and other products to prevent and treat life-threatening bacterial infections.” Specifically, it invests in companies that target the bad bugs on the CDC and WHO priority lists.

Among its 30-plus antibacterial project investments, for example, is a Bangalore, India startup called Bugworks Research that has raised $9 million, not including grant money from CARB-X. Bugworks’ leading candidate is a compound called GYROX, which is being developed as an intravenous and oral treatment for multi-drug resistant infections. The new antibiotic is able to bypass some of the normal bacterial defenses to get at the heart of the superbug for the fatal blow. The company is expected to start clinical trials of GYROX next year.
Money is also flowing from other places. For instance, earlier this year, Novo Holdings, which is related to the Novo family of independent companies that includes pharmaceutical giant Novo Nordisk (NVO) and Novozymes (NZYMB) announced it would create a new venture fund targeting “startups, early-stage companies and corporate spin-outs” that were tackling drug-resistant superbugs. Reuters reported the $165 million Repair Impact Fund would dole out between $20 million and $40 million per year over a period of three to five years.
Pharmaceutical Companies and the Superbugs War
Earlier this year, the Access to Medicines Foundation published a new index called the Antimicrobial Resistance Benchmark that rated the top 30 companies engaged in the war on superbugs, split into three broad categories – big pharma, generic drug makers and mostly small cap biopharmaceutical companies.

GlaxoSmithKline (GSK) topped the list as the pharmaceutical company leading the charge against superbugs, as it is the “largest investor in the space of antimicrobial R&D and has a promising pipeline in terms of size as well as the number of vaccines and novel antimicrobial candidates.” How big? GSK has 55 antimicrobial R&D projects in its pipeline, 28 of which are in clinical stage development. Forty of the company’s projects target priority pathogens identified by CDC and/or WHO. For example, GSK is working on nearly a dozen vaccines in everything from Shigellosis (caused by Shigella bacteria, one of the main culprits behind Montezuma’s Revenge or Delhi Belly) to a version of its meningitis vaccine to protect against gonorrhoea, which is from the same bacterial genus.
The benchmark pegged a company called Entasis (ETTX) as the best of the biopharmaceutical bunch. Based outside of Boston and founded in 2015, Entasis just joined the NASDAQ last month, raising $75 million in an IPO after taking in about $128 million from various investors, including both CARB-X and Novo Holdings. It has a market cap barely treading above $100 million, after being valued at nearly twice that much pre-IPO.
The company’s fortunes are riding on a handful of drugs in its pipeline, including one called Zoliflodacin, an oral antibiotic for treating gonorrhea, which is one of the most common STDs, with about 800,000 people in the United States infected each year – about the same as herpes. But worse.
Startups and the Superbugs War

Other startups are turning away from antibiotics altogether. For instance, Adaptive Phage Therapeutics out of Washington, DC has raised $3.1 million (most of it in debt financing) to develop a platform that uses machine learning to determine which killer virus (called a phage) would be best suited to infect and destroy a particular bacteria. The idea is to eventually automate the process so that a hospital could dispense the right phage within minutes, according to MIT Technology Review.
Conclusion
These are just a few of the emerging technologies being moved to the front lines in the war against the superbugs. Elsewhere, researchers are working on a material, which could be applied to gauze to wrap a wound, that would prevent the biofilm that clumps bacteria together from forming. IBM researchers are working on a synthetic molecule that latches onto bacterial cells to kill them. And researchers in Australia propose starving the bacteria of needed iron. The incentive to come up with the next super solution – millions of lives, billions of dollars – could emerge within just the next few years, based on the current frenzy. Hopefully, we can go back to worrying about the mundane stuff like killer zombies and planet-destroying space rocks.
Sign up to our newsletter to get more of our great research delivered straight to your inbox!
Nanalyze Weekly includes useful insights written by our team of underpaid MBAs, research on new disruptive technology stocks flying under the radar, and summaries of our recent research. Always 100% free.














